- An overdistended uterus is unable to produce efficient contractions
- Drain the excessive fluid
- By rupturing the membranes
- Risk of cord prolapse if cervix is open more than a finger
- By external drainage with an i.v. cannula
- No risk of cord prolapse
- By rupturing the membranes
Tag: dr erik erichsen
POST PARTUM HEMORRHAGE (PPH)
Causes:
- Atony of the uterus
- Retained placental parts
- Uterine rupture
- Cervical and/or vaginal tears
- DIC (HELLP)
Treatment:
- Resuscitate with fluids
- Massage the uterus manually
- Apply firm and continuous pressure suprapubically with a closed fist for a full 10 minutes
- Eyes on the watch!
- Oxytocin infusion i.v. (preferred)
- 30 units in 500 cc in Normal Saline
- Infused over 2 to 4 hours
- Misostoprol (Cytotec) tablets (if oxytocin is not available)
- 2 – 4 tablets
- Oral or rectal adminstration
- 2 – 4 tablets
Bleeding does not subside:
- Bring patient to operating theater
- Place legs in stirrups
- Examine by intracavitary palpation
- Placental parts present:
- Remove
- Uterine rupture present:
- Laparotomy and repair
- Neither retained placenta nor rupture of the uterus is present:
- Pack firmly with gauze
- Remove gauze pack in the operating theater after 24 hours
- Placental parts present:
- Transfuse one or two units of fresh blood
- Perform hysterectomy as a last resort
Speculum Examination:
- It is usually difficult and messy to identify bleeding site(s) from cervical tears
- Attempts to suture the friable tissue results in further tearing and bleeding
- Proceed directly with gauze packing in the absence of retained placental parts or ruptured uterus.
RETAINED PLACENTA
Early presentation:
Induce delivery of the retained placenta:
- Nitroglycerine sublingually or nasally
- Misostoprol (Cytotec)
- Oxytocin
Late presentation:
Manual or instrumental removal:
- Introduce one hand into the uterus
- Use the ulnar border of the intrauterine hand to dissect the placenta from the uterine wall
- Apply contra pressure on outside of the uterus with other hand on abdomen
- In case a closed or closing cervix does not allow the entire hand to enter the intrauterine cavity, two fingers are usually sufficient
- If not, use instruments
- A large sponge forceps (ring forceps) will do
Very late presentation with severe anemia and/or sepsis:
Supravaginal (subtotal) hysterectomy.

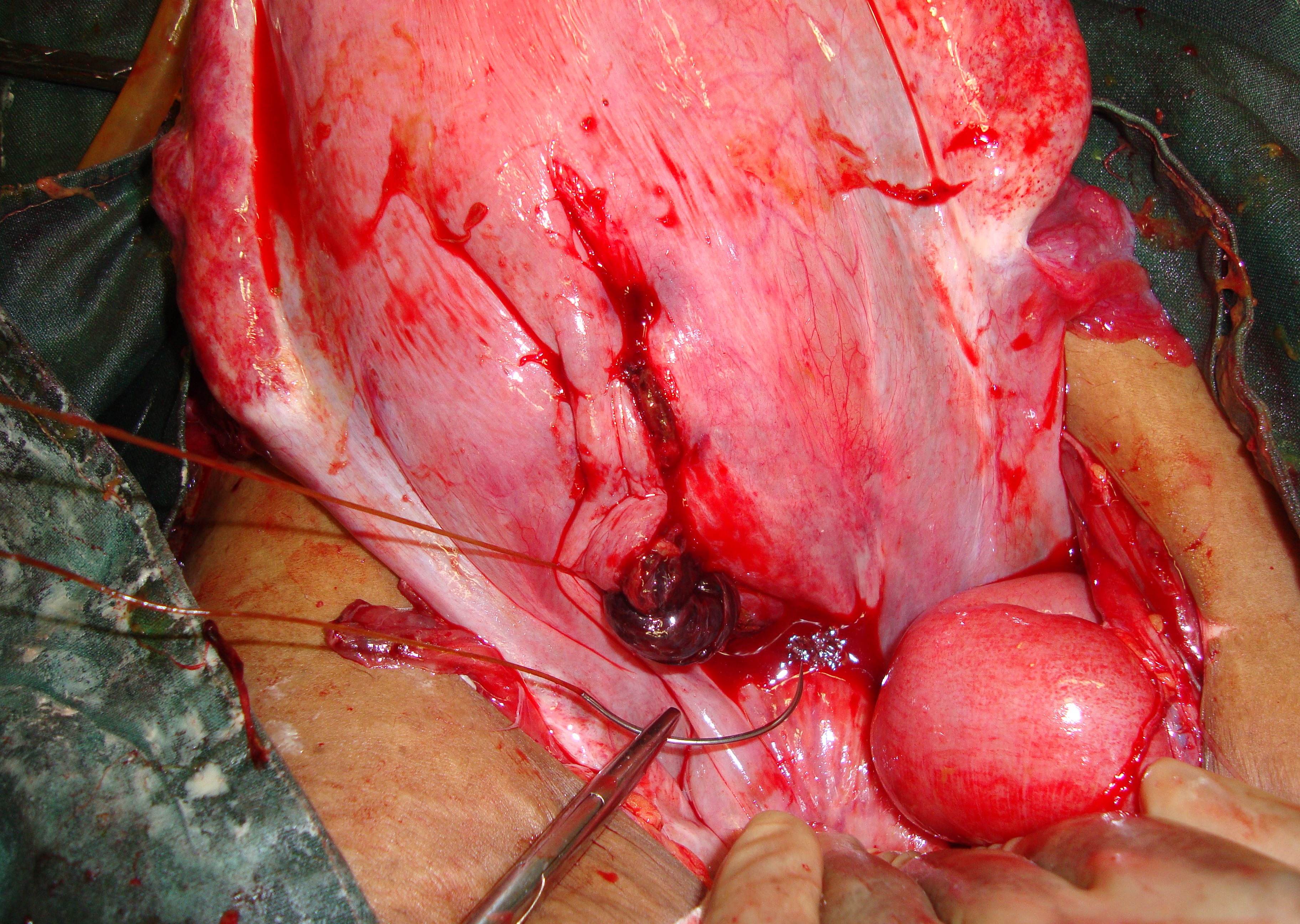
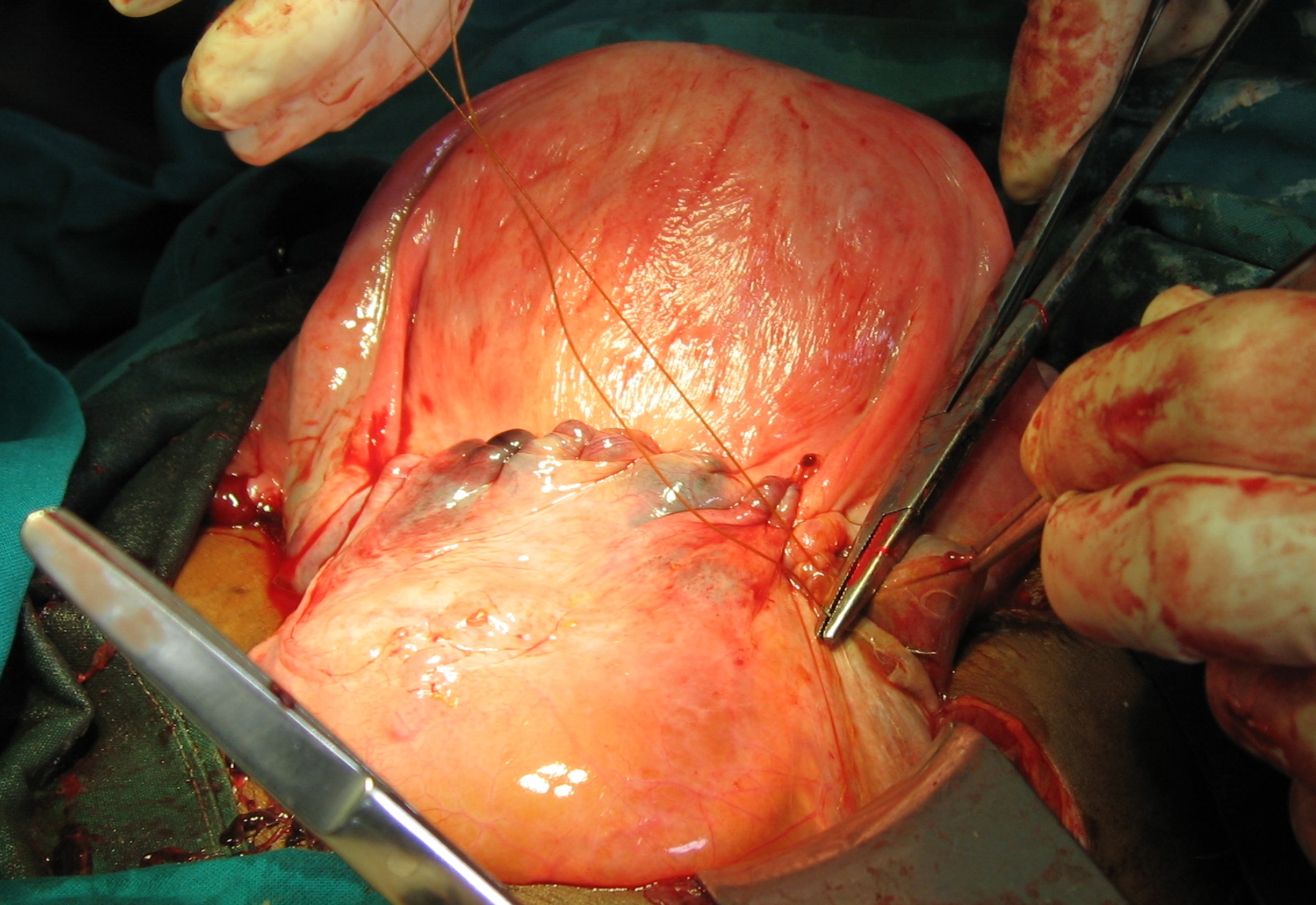
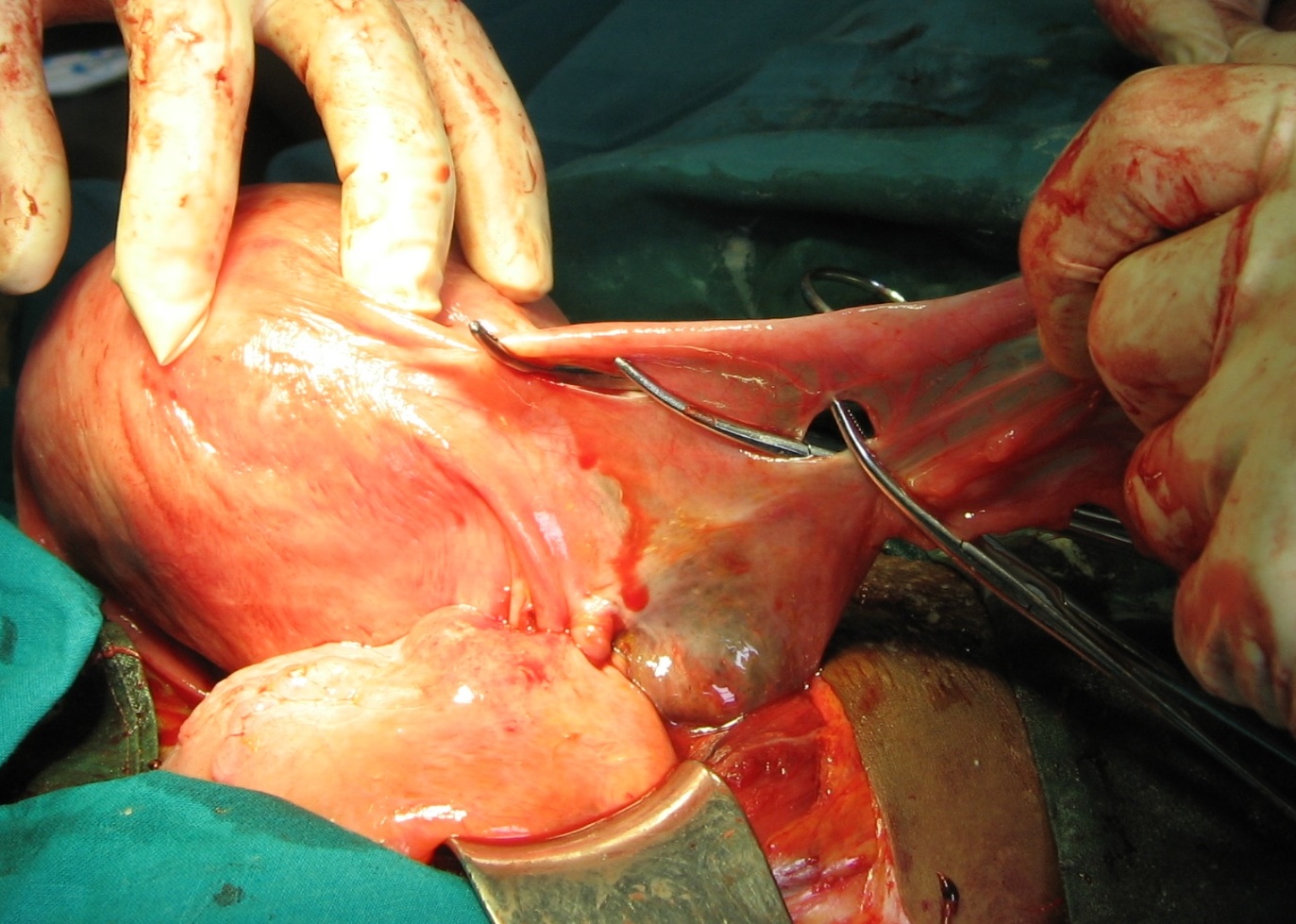
Supravaginal (subtotal) hysterectomy with retained placenta. Uterus pale due to severe anemia
SHOULDER DYSTOCIA
- Do not panic
- Do not use forceful traction on head
- May cause severe damage to both child and mother
- Go systematically through following steps:
- Wipe baby’s face clean
- Keep airways free
- Use suction to remove mucus and meconium
- Make a generous episiotomy.
- This alone might solve the problem
- Apply Loevset’s maneuver
- Grasp lateral border of the scapula with four ulnar fingers of your hand
- Rotate truncus 180°
- Use right hand when the back is turned to the (mother’s) left and vice versa
- As the birth canal is shorter anteriorly bringing the posterior shoulder anteriorly may deliver it
- Repeat the maneuver
- Fracture both clavicles
- Decreases the overall dimension of the shoulders
- Place the delivery hook under one axilla
- Apply traction
- Rotate truncus 180° (Loevset’s Maneuver)
- Perform symphysiotomy
TRANSVERSE PRESENTATION
Transverse presentation is often accompanied by arm prolapse (compound transverse presentation).

Compound transverse presentation
Alive fetus
Neglected compound transverse presentation
Dead fetus
GESTATIONAL AGE < 32 WEEKS / WEIGHT < 1500 GRAM
- Vaginal delivery
GESTATIONAL AGE > 32 WEEKS / WEIGHT > 1500 GRAM
ALIVE FETUS
- Cervix closed:
- Cesarean Sectio
- Cervix closed and membranes intact:
- External Version
- Cervix fully dilated / Membranes ruptured recently / Contractions not very strong:
- Internal version and extraction using one or both feet
- Introduce one hand in uterus
- Search for small parts of the fetus
- Identify one or both feet
- Foot has a heal
- Hand has a thumb
- Grasp one or both feet with forked fingergrip from behind
- Apply strong traction on the foot/feet
- Rotate the fetus with a combination of
- Traction on foot/feet
- Upward pressure on caput with other hand on mother’s abdomen
- Continue strong traction on foot/feet
- Combined with pumping movements
- Grasp front of knee with the other hand
- Extract the upper part of body by a combination of
- Strong traction
- Pumping movements
- Grasp pelvis with both hands
- Extract upper part of body by a combination of
- Strong traction
- Pumping movementsRelease arms
- Deliver head by Mauriceau-Levret’s maneuver
- Internal version and extraction using one or both feet
DEAD FETUS
- Destructive delivery
- Decapitation
- Exvisceration
BETWEEN 32 – 34 WEEKS / 1500 – 2500 gram
Relay on your own judgement
TRIAL OF SCAR / PREVIOUS C/S
Repeat C/S whenever there is a scar after a previous one
- Vaginal delivery after previous C/S – “Trial of Scar” – is risky
- The scar from previous C/S may easily burst
- High risk of uterine rupture
- Do not perform vaginal delivery
- Unless monitored continuously and closely
- Staff member at bedside assigned exclusively for that purpose

Not recommended 
Not recommended
URINARY RETENTION
If catheterization of a full bladder fails:
- Try to insert a rigid catheter
- Try to insert a metal catheter
- Perform a suprapubic puncture with a wide bore needle.
UTERINE RUPTURE
Ultimate result of unrelieved obstructive labor
Symptoms and signs
- Shock
- Abdominal pain
- Contractions absent
- Fetal heartbeats absent
- Small parts of fetus are visible and/or palpable directly under the skin
Diagnosis
- Usually straight forward
- Occassionally challenging
- Particularly with posterior ruptures
- Abdominal aspiration:
- Blood at aspiration confirms the diagnosis
- No blood at aspiration is inconclusive
If diagnosis is still in doubt, there are two options:
I. Do a laparotomy
Rupture is present:
- Proceed with repair
No rupture is present:
- Close the abdominal incision
- Perform destructive delivery

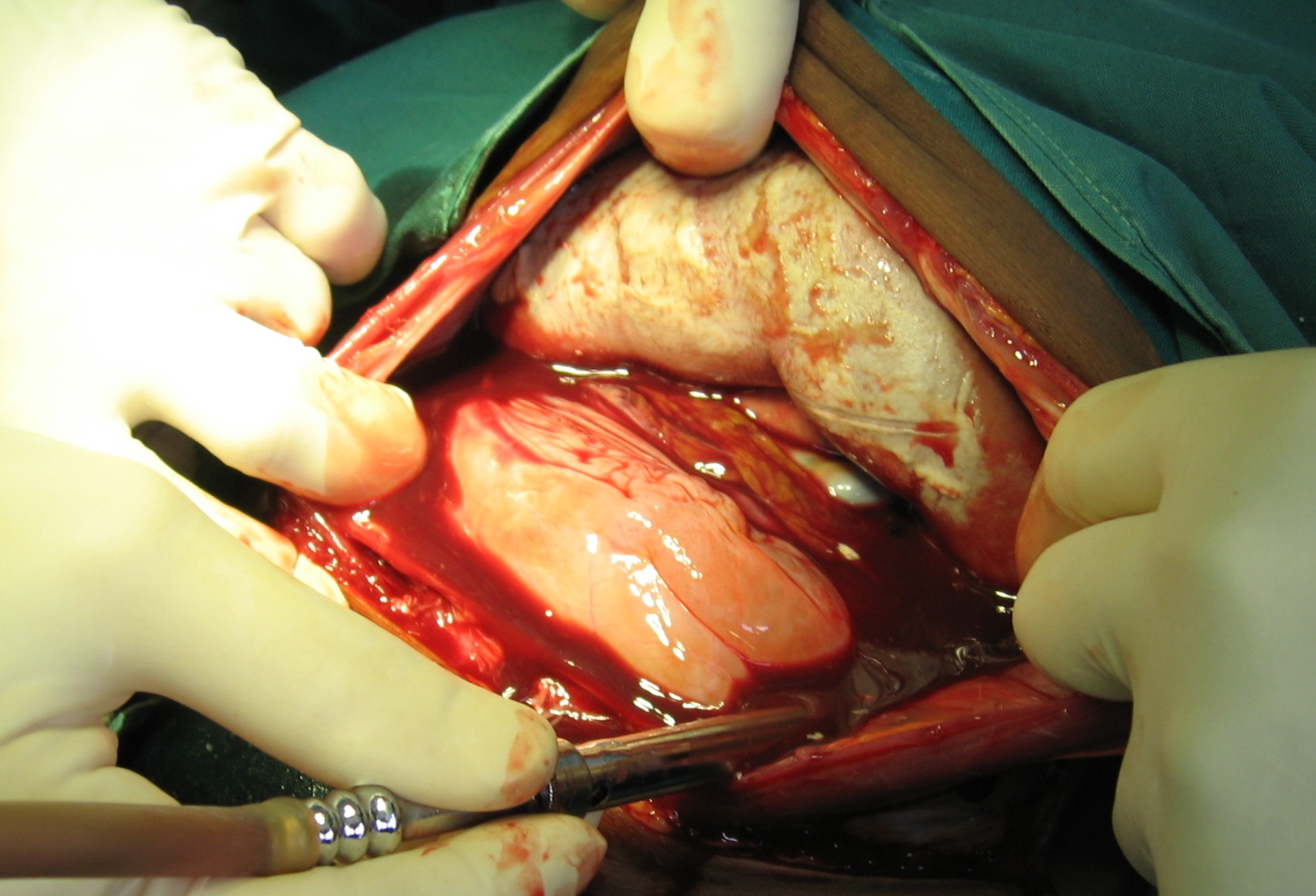
Suspected rupture 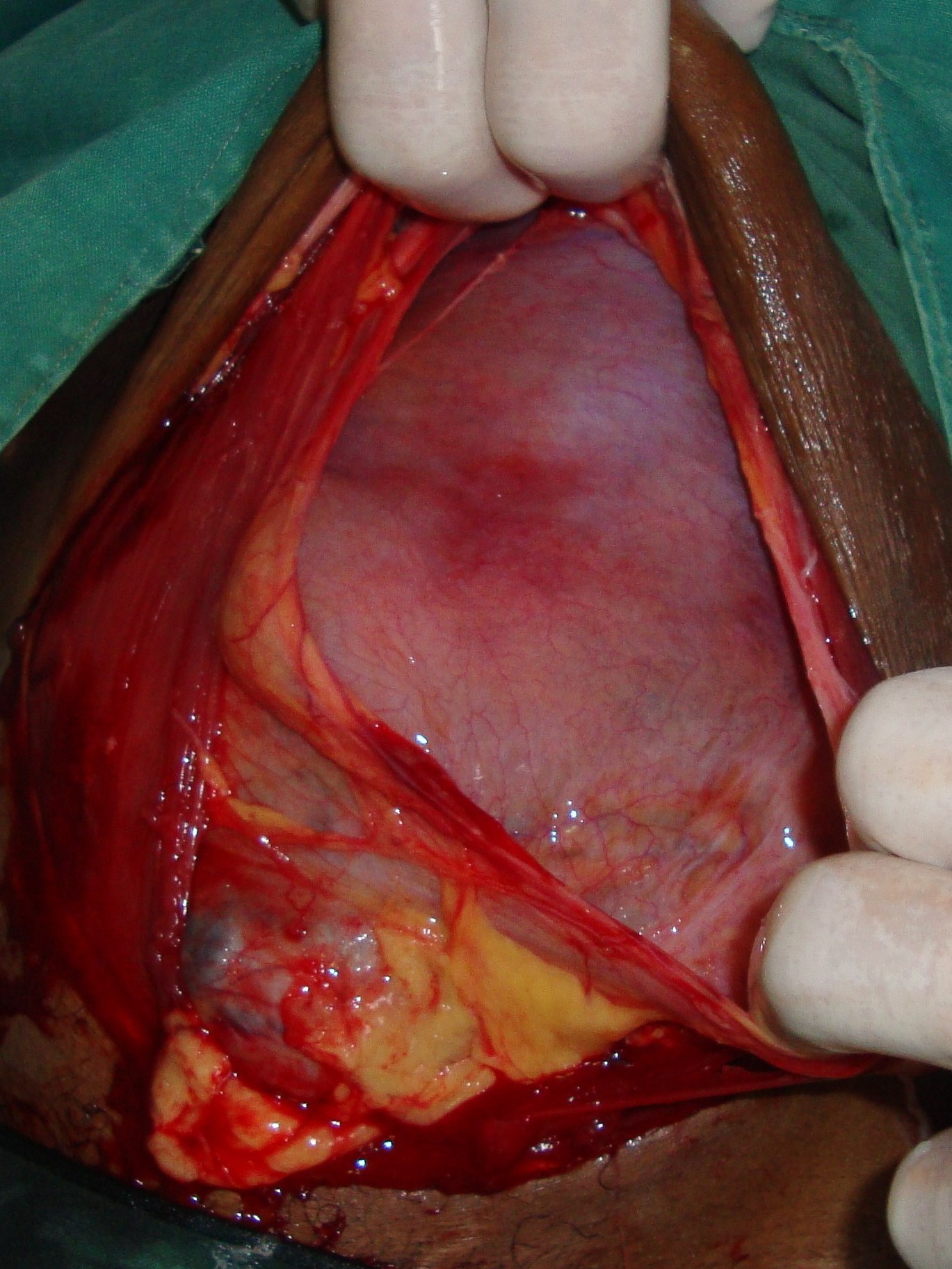
No rupture at laparotomy 
Prepare for destructive delivery 
II. Deliver the dead fetus by destructive procedure
Check uterine cavity manually for rupture
- Rupture is present
- Proceed with laparotomy & repair
In selected cases, when:
- Peritoneum is intact
- The palpating hand does not come into direct contact with the bowels
- Patient is critical
- Surgeon unexperienced
- Relay on firm gauze packing
- Remove pack in OR after 24 hours
TYPES of RUPTURES:
- Anterior – transverse or longitudinal – with or without bladder rupture
- Lateral – always longitudinal – with or without bladder rupture
- Posterior – transverse or longitudinal – always without bladder rupture
The far most common type is the anterior transverse.
Use the same principles as in trauma surgery:
- Minimal Surgery
- Make a fast and simple repair of the rupture
- Do not traumatize the patient further by performing hysterectomy.
- The only indications for hysterectomy are:
- Gangrene of the uterus
- When technically easier and faster to do than a repair

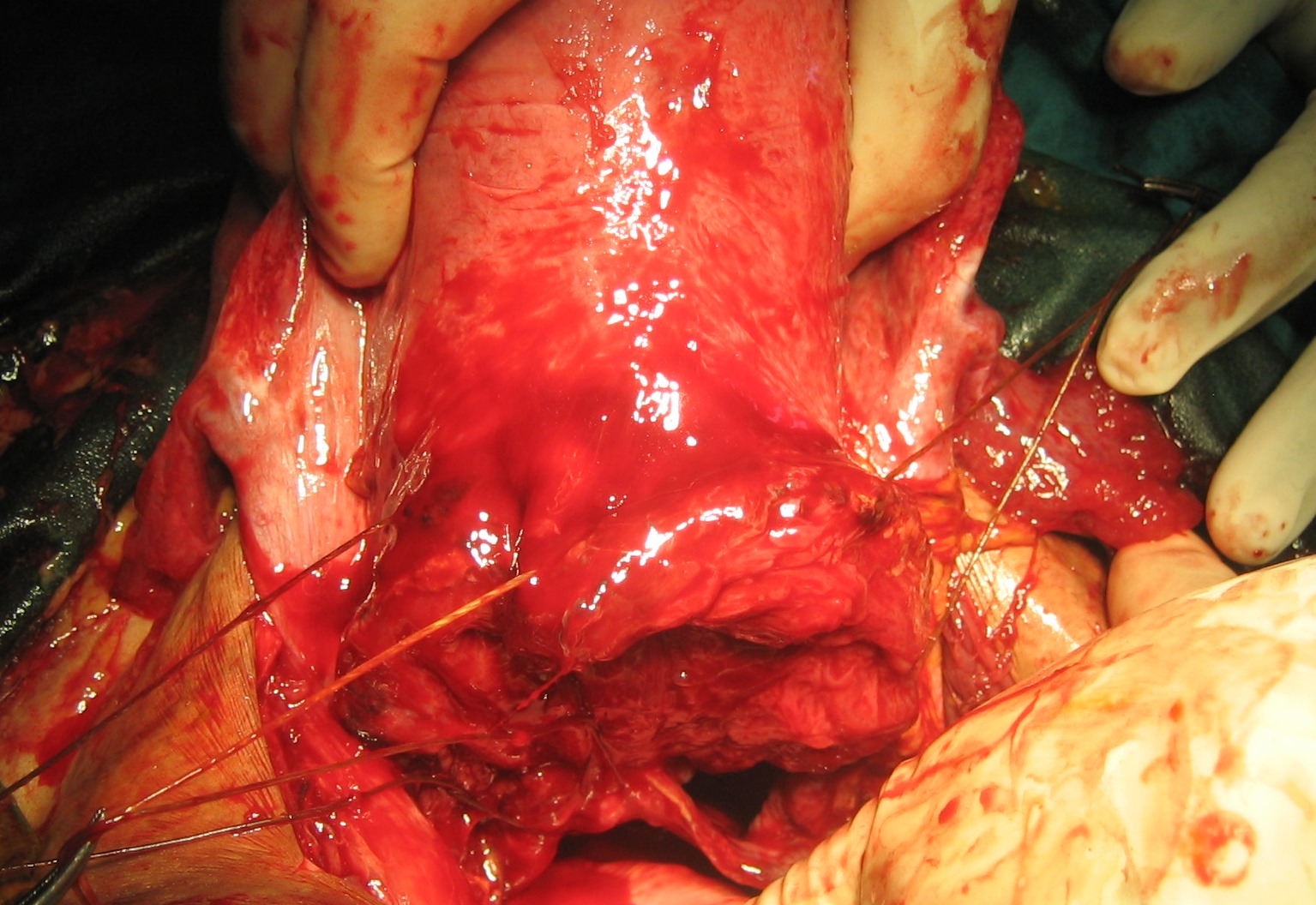
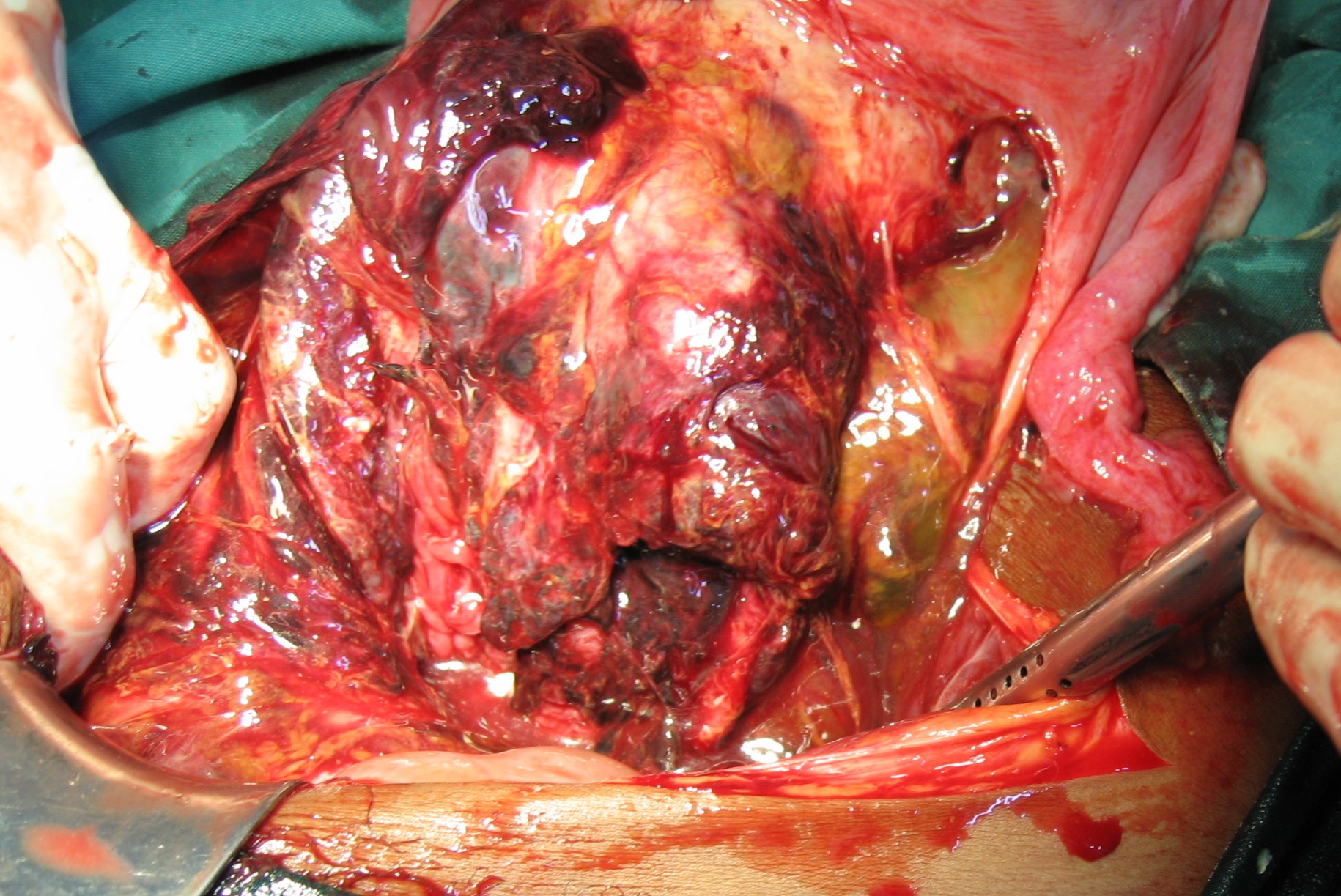
Gangrenous uterus

Extensive rupture 

Uterus removed
REPAIR OF RUPTURED UTERUS
- Main objectives of the repair are to:
- Stop bleeding
- Separate the abdominal cavity from vagina
SURGICAL TECHNIQUE
- Resuscitate with i.v. fluids
- Give i.v. antibiotics (ampicillin/gentamycin/metronidazole)
- Transfuse one or two units of fresh blood if available
- Ketamine i.v. works well
- General anesthesia is even better when a skilled anesthetist is present
- Repair the rupture with a continuous inverting suture
- Use heavy resorbable suture (Chromic Catgut or Polyglycolic Acid)
- Cover the repair with a second layer of peritoneum
- In critical situations suturing the torn peritoneum may be sufficient and lifesaving.
- Reaching the most distal part of a rupture may be challenging.
- Do not struggle
- Leaving the most distal part of the rupture open for drainage is in fact an advantage.
- In case the patient has no – or only one – living child
- The relatives promise solemnly to take her to hospital for C/S at the next delivery
- Offer that option.
- Otherwise perform bilateral tubal ligation (BTL).
- Clean the abdominal cavity
- Remove all contaminated, infected blood
- Irrigate with plenty of saline before closure.
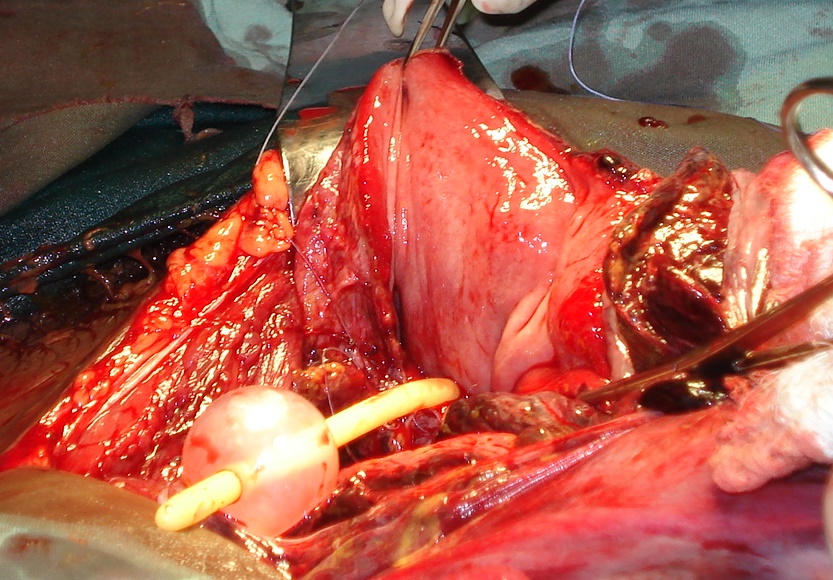
REPAIR OF ANTERIOR TRANSVERSE UTERINE RUPTURE











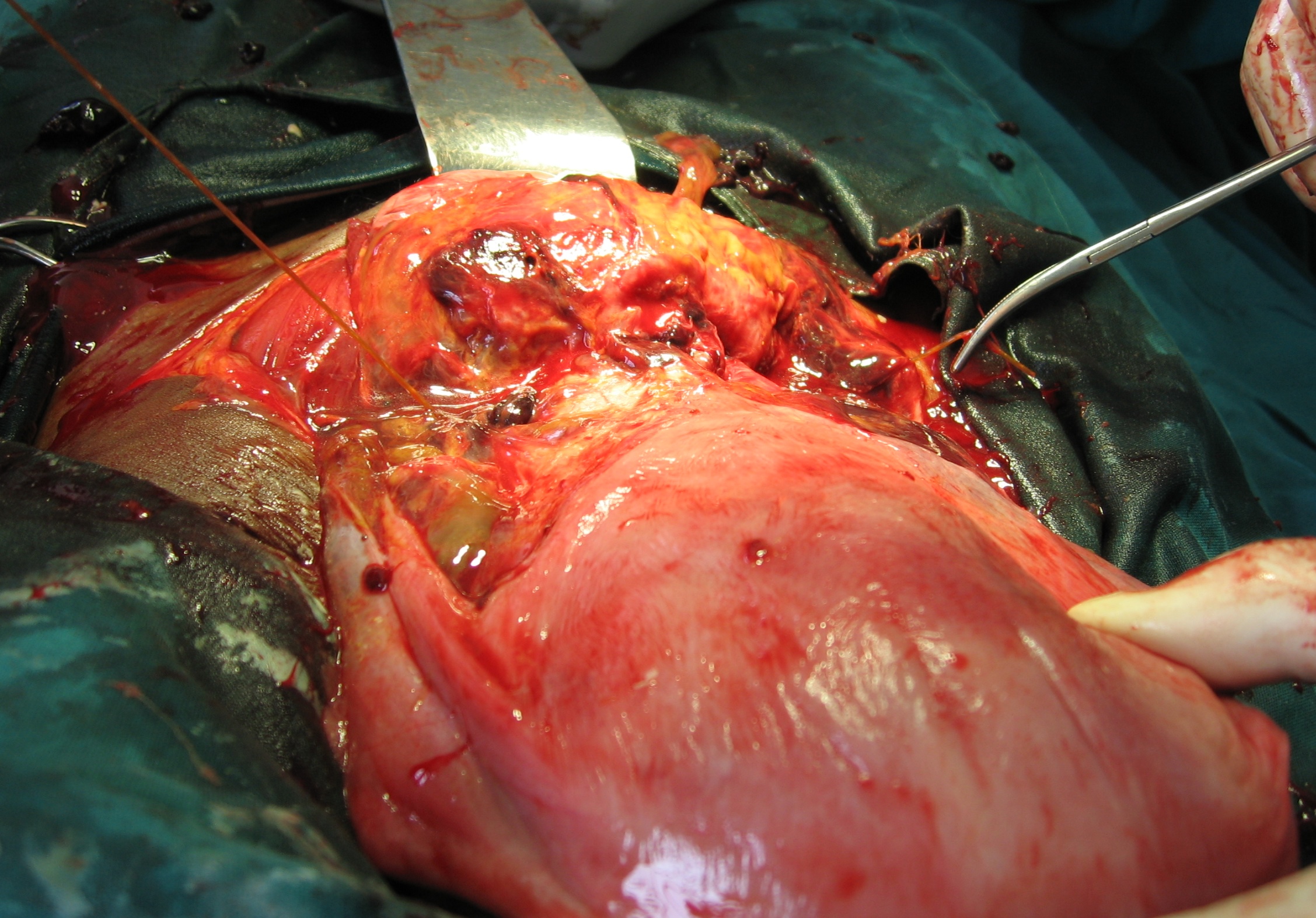
Salpingectomy/BTL 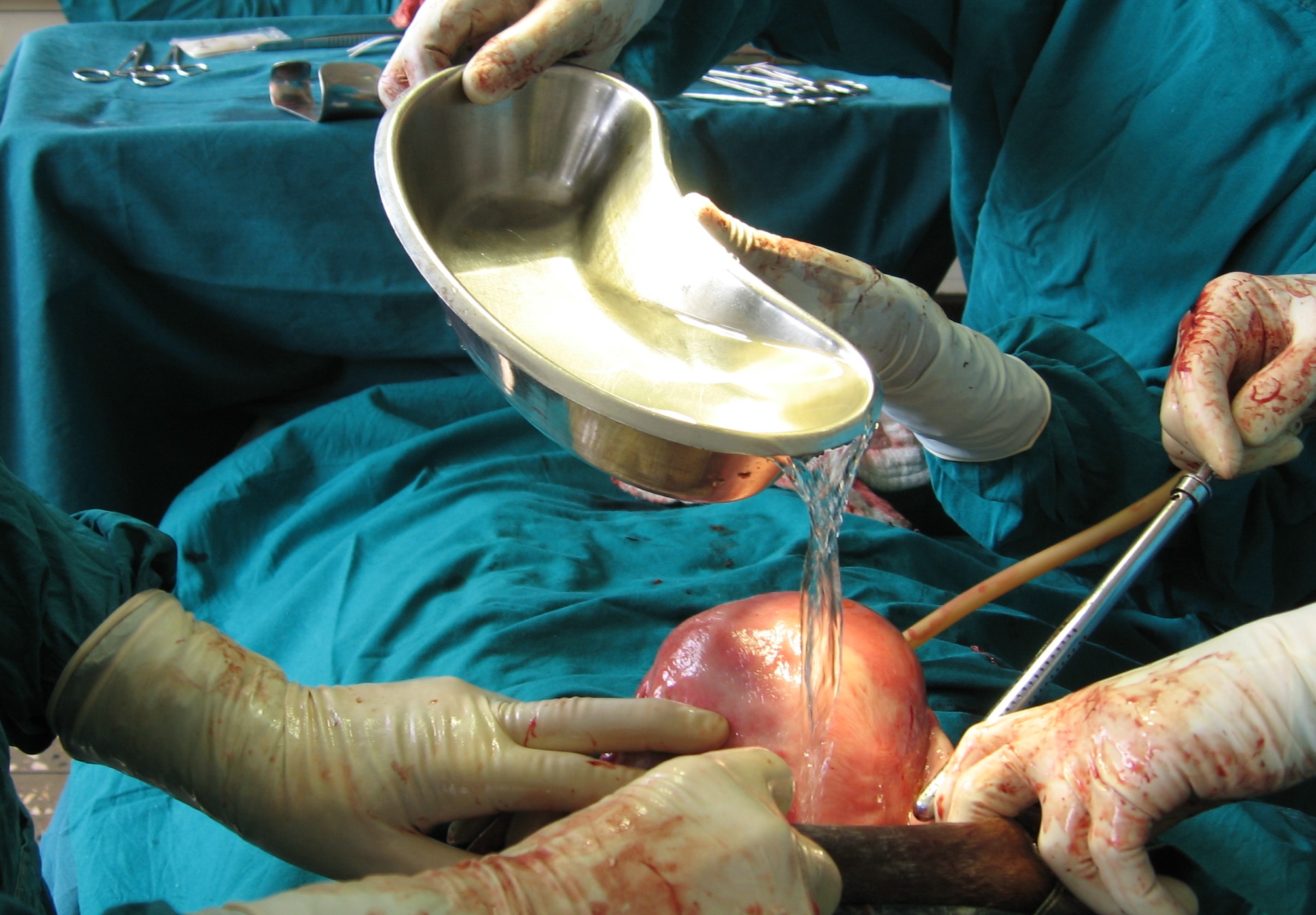



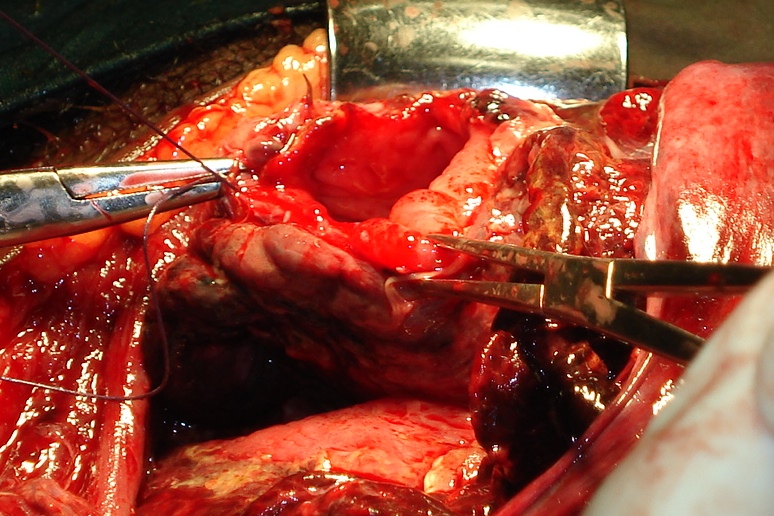
REPAIR OF LATERAL UTERINE RUPTURE
- Close rupture with a continuous suture
- Leave the most distal part of the rupture open for drainage
- Cover the repair with a second layer of peritoneum



First layer 

Leave the very distal part of the wound open for drainage 

Second layer 

REPAIR OF POSTERIOR LONGITUDINAL
- Same technique as for lateral rupture
- A second layer is usually not possible
REPAIR OF POSTERIOR TRANSVERSE RUPTURE
- Somewhat challenging as the lower segment is short and inaccessible.
- Repair with interrupted inverting sutures in a row
- Tie suture when all are in place
REPAIR OF RUPTURED BLADDER
Bloody urine raises the suspicion of bladder involvement
SURGICAL TECHNIQUE
- Repair bladder with one or two layers of continuous inverting resorbable suture
- Watch out for the ureters
- Repair the ruptured uterus
- In critical situations the bladder can be left unrepaired with an indwellingath catheter
- The resulting VVF (vesicovaginal fistula) can be repaired later
Using these principles resulted in the present maternal mortality of less than 3 % in Aira Hospital as seen in the presentation below. One of the two deceased patients in the material expired before reaching the operating theater. The maternal survival rate after surgery is thus 98.6 % and mortality with surgical treatment 1,4 %
An improvement from 5% mortality previous 10 years
An improvement from the 5 % mortality rate during the preceding 10 years.
VACUUM EXTRACTION
A silicone cup is the best choice

- Easier to apply than the original metal cup
- Traction can be started immediately after applying vacuum
- No need to wait until a caput has built up
Technique:
- Extraction must be synchronous with the contractions
- Abort extraction if the cup slips more than twice
- Abort extraction if not succesfull within 15 min
- Severe damage may otherwise be the consequence